NMR based lipoprotein subclass analysis for assessing the effect of dietary cheese fat on blood cholesterol Introduction*
Cardiovascular disease is the leading cause of death worldwide, accounting for 31% of all global deaths. Poor cardiovascular health is also a major cause of morbidity arising from heart attacks, strokes, heart failure, chronic kidney disease, and the onset of vascular dementia. There have consequently been considerable global efforts to improve cardiovascular health. There is considerable evidence showing that reducing plasma cholesterol levels can lead to clinically relevant reductions in the risk of developing cardiovascular disease1. A key target for reducing the prevalence of cardiovascular disease has thus been reducing dietary intake of saturated fat and increasing the prescription of prophylactic statins1,2. However, although a high plasma concentration of low-density lipoprotein (LDL) cholesterol is one of the main risk factors for developing cardiovascular disease, there is an increasing prevalence of cardiovascular disease among individuals with plasma concentrations of LDL-cholesterol that are wit in the normal range3. It appears that this is because the size, density, and physiochemical properties of LDL-cholesterol particles, and not just the absolute concentration of LDL-cholesterol, can affect cardiovascular disease risk4. The effects of diet on the type of LDL-cholesterol present in the blood are therefore being studied to determine which diets increase the risk of cardiovascular disease.
Blood cholesterol and cardiovascular risk
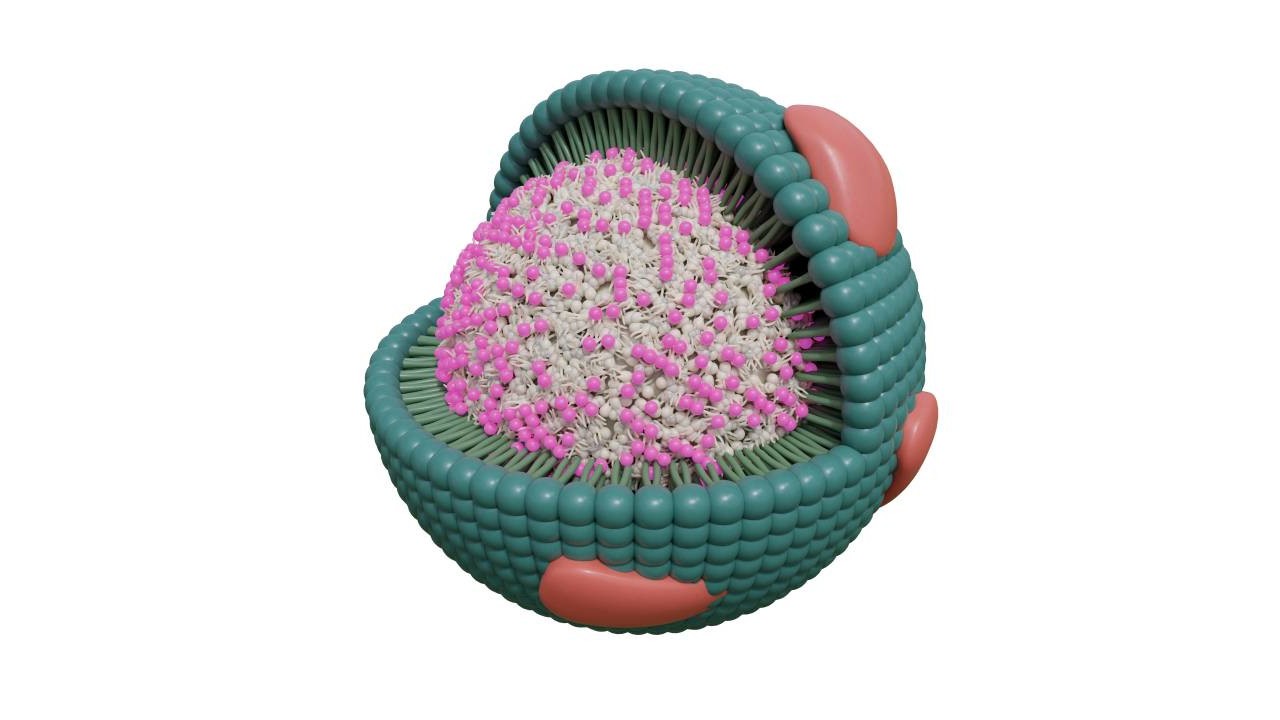
Cholesterol is essential for maintaining the integrity of animal cell membranes and is a component of several vital hormones. The liver typically produces adequate cholesterol to meet the requirements for these important functions. If there is excessive additional dietary cholesterol, this can be detrimental to cardiovascular health.
However, the health impact of excess circulating cholesterol is related to whether it is being carried as high-density-lipoprotein (HDL) cholesterol or LDL-cholesterol. Excess LDL-cholesterol can stick to the lining of arteries—atherosclerosis—impeding blood flow and increasing the risk of cardiovascular disorders. In contrast, HDLcholesterol generally prevents the build-up of LDL-cholesterol, thereby reducing the risk of cardiovascular disease.
Measurements of plasma LDL-cholesterol levels have been used as an indicator of cardiovascular risk for many years and statins are commonly prescribed to patients deemed to be at high risk due to elevated levels of circulating LDL-cholesterol. Recently, however, it has become apparent that cardiovascular risk is not determined solely by the concentration of LDL-cholesterol, but also by the size of the particles of LDL-cholesterol5. Small, dense LDL (sdLDL) particles are associated with a higher risk of cardiovascular disease irrespective of LDL-cholesterol concentration6.
Studies have shown that the size of LDL-cholesterol particles varies with diet. Interestingly, dietary saturated fatty acids that are associated with high cardiovascular risk were associated with large, buoyant, lower risk LDL-cholesterol7. Further, research is needed to define the cardiovascular risk associated with fat intake.
Effects of cheese on blood cholesterol
Patients at high risk of cardiovascular disease are commonly recommended to limit cheese intake due to its high saturated fat content. However, several studies have reported that cheese does not affect either plasma cholesterol levels or cardiovascular risk8.
It is possible that these unexpected findings could be explained by the fact that the saturated fat in cheese results in the formation of larger LDL-cholesterol particles that carry a lower risk of developing cardiovascular disease. Such a hypothesis was recently tested by researchers in Denmark who compared the effects of regular-fat cheese, reduced-fat cheese and carbohydrate-rich foods on LDL particle size distribution9.
Adult patients with = 2 metabolic syndrome risk factors were randomly allocated to receive a diet that included regular-fat cheese (REG), reduced-fat cheese (RED) or additional carbohydrate (CHO) instead of cheese for 12 weeks. Fasting blood samples collected at baseline (week 0) and after 12 weeks were analyzed by 1H NMR using a Bruker Avance IVDr 600 MHz system and the LDL particle size distribution, cholesterol concentration and more than 100 other lipoprotein parameters were determined using the Bruker IVDr Lipoprotein Subclasses Analysis (B.I.LISA) module.
Regular-fat cheese did not increase either the number or size of LDL-cholesterol particles compared with reduced-fat cheese9. Furthermore, there were no significant differences in body weight, fat mass, lean body mass, waist circumference, or blood pressure between REG and RED diets or between the REG and CHO diets. There were also no significant differences in the concentrations of cholesterol in the different lipoprotein subclasses between the diets. The lack of difference in LDL particle size between the two cheese groups was unexpected, as the saturated fat intake in the regular-fat cheese group was significantly higher than in the reduced-fat cheese group.
An analysis by gender revealed that, compared with the RED diet, the REG diet decreased total LDL particle count in men. In women, the number of high-risk sdLDL-cholesterol particles was increased with the REG diet compared with the CHO diet.
These latest data suggest that the lipoprotein response to cheese intake is gender specific. The study also showed that the intake of regular-fat cheese did not alter LDL-cholesterol particle size distribution compared to reduced-fat cheese after a 12-week intervention. Further investigation is required to assess gender differences in cholesterol levels after cheese consumption and to evaluate whether the size of LDL-cholesterol particles may be a better predictor of cardiovascular risk than LDL concentration.
References
1. Scandinavian Simvastatin Survival Study Group. Lancet 1994;344:1383–9.
2. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Circulation. 002;106:3143–421.
3. Genest JJ, et al. Am J Cardiol. 1991;67:1185–1189.
4. Krauss RM, Burke DJ. J Lipid Res. 1982;23:97–104.
5. Krauss RM. Arterioscler Thromb Vasc Biol. 2014;34:959–961.
6. Mora S, et al. Circulation. 2015;132:2220–2229.
7. Dreon DM, et al. Am J Clin Nutr. 1998;67:828–836.
8. Chen G-C, et al. Eur J Nutr. 2016;56:2565–2575.
9. Raziani F, et al. Nutrition & Metabolism 2018;15:61.
https://doi.org/10.1186/s12986-018-0300-0
* Bruker NMR Instruments are for research Use Only. Not for Use in Clinical Diagnostic Procedures.