Lipoprotein Markers May help Identifying and Predicting Disability Status in Patients with Relapse-Remitting Multiple Sclerosis*
Lipoprotein Markers May help Identifying and Predicting Disability Status in Patients with Relapse-Remitting Multiple Sclerosis
Multiple sclerosis (MS), a chronic neuroinflammatory disorder associated with non-traumatic acquired disability, affects more than 2.2 million people across the world. Since 1990, the global prevalence of MS has risen approximately 10.4%. Despite this increase, unmet treatment needs for this disorder still exist, particularly for patients with relapsing-remitting MS (RRMS), the most common type of MS characterized by frequent disease relapses with alternating periods of remission.
Markers of Progression and Disability
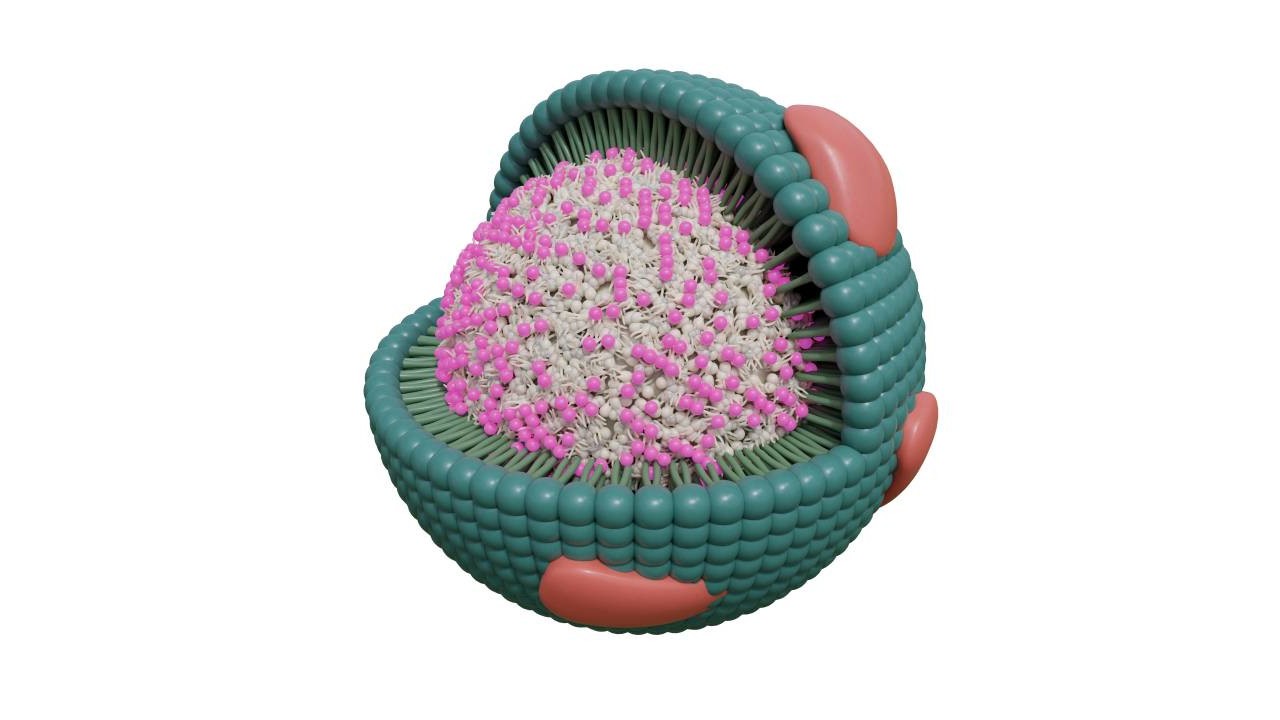
Intensive clinical measures and serial brain imaging are the most common techniques used for monitoring progression of MS. Blood markers of progression, while currently non-existent, may be helpful for more accurate risk stratification and treatment efficacy monitoring. Inflammatory markers and lipids are potential biomarkers, as some studies have previously demonstrated an association between dyslipidemia and increased MS activity, including new magnetic resonance imaging lesions and worsening disability.
Other studies have found that patients with MS can be distinguished from non-MS healthy controls by concentrations of cholesterols, fatty acids, triglycerides, and phospholipids. These studies also suggest that some lipids can distinguish patients with MS in terms of the degree of clinical disability or disease stage.
1H-NMR based lipoprotein subclasses analysis Study Examines Markers of MS Disability
In a recent study using NMR spectroscopy to quantify lipids and lipoproteins, researchers from Oxford University and Imperial College London found relationships between disability, inflammatory responses, and systemic lipid metabolism in patients with RRMS relative to healthy controls. Specifically, concentrations of lipids within very low-density lipoprotein (VLDL) sub-fractions, including free cholesterol and triglycerides, were associated with worsening disability and pro-inflammatory markers in plasma of patients with RRMS. Based on their findings, the researchers also concluded that immune activation in the disease may be attributable to systemic inflammation.
The study included 27 patients with RRMS with a median Expanded Disability Status Scale (EDSS) score of 1.5 (range, 1–7). Additionally, 31 healthy volunteer controls were included as a comparison. Participating patients, recruited from the Imperial College Healthcare NHS Trust, were included in the study prior to initiation of a new disease-modifying therapy.
Researchers obtained non-fasting venous blood samples at each study visit in EDTA tubes. Within 3 hours of sample collection, samples were centrifuged at 1400 × g for approximately 10 minutes to get plasma samples.
Prior performing the NMR spectroscopy analysis, the investigators centrifuged plasma samples for 5 minutes to remove solid particles.
1H-NMR spectra were acquired using a Bruker Avance IVDr 600 MHz system and samples were prepared according to standard procedures and measured in full automation with the Bruker’s bodyfluid NMR methods package. Bruker’s B.I.LISA lipoprotein module was used to perform plasma lipoprotein quantification. Using this method, the researchers estimated total plasma triglyceride, cholesterol, free cholesterol, phospholipid, and apolipoprotein A1, A2, and B. Concentrations of these lipids were also estimated within VLDL, intermediate-density lipoprotein, low-density lipoprotein, and high-density lipoprotein classes. The MesoScale Discovery V-PLEX kit was used to measure plasma cytokines.
A total of 23 lipids within the VLDL and HDL sub-fractions were significantly increased in the patients with MS versus healthy volunteers (p<0.05). In the multivariate regression model, there was a high significant correlation between lipids within VLDL sub-classes and the EDSS (p<0.05). An optimal model for EDDS, which was based on the Akaike Information Criterion, included free cholesterol carried by sex, VLDL-2, and age (R2 = 0.38; p<0.05). In contrast, this model excluded disease duration, body mass index, and cholesterol. This model featured a moderate correlation for EDDS (R2 = 0.37; p=0.0001). Free cholesterol, when included in the model, was independently significant (p=0.003). Additionally, the investigators found a high correlation between free cholesterol carried by VLDL-2 with plasma cytokines CCL-17 and IL-7 (R2 = 0.78; p<0.0001).
Limitations of the study were the inclusion of non-fasting samples, its cross-sectional nature, lack of a validation group, and a small sample size. The researchers also mention that they did not match patients with healthy controls for diet, which may further limit the findings.
Potential Implications for Future Research and Clinical Practice
Despite these limitations, this study, which relied on NMR based metabolomics , suggests that the action of decreasing plasma lipid concentrations and subsequent monocyte activation may help lipid-lowering drugs achieve clinical benefit in patients with inflammatory diseases, including RRMS. Further prospective studies may help explain how lipid concentrations within various VLDL sub-classes change during the course of MS. These studies may also help identify the prognostic value of lipid-lowering measures in the prediction of disability and its progression in RRMS.
References:
• Gafson AR, Thorne T, McKechnie CIJ, et al. Lipoprotein markers associated with disability from multiple sclerosis. Sci Rep. 2018;8(1):17026.
• Bruker Avance III 600-I. University of California San Francisco. https://pharm.ucsf.edu/nmr/instruments/bruker-600.
• GBD 2016 Multiple Sclerosis Collaborators. Global, regional, and national burden of multiple sclerosis 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(3):269-285.
* Bruker NMR Instruments are for research Use Only. Not for Use in Clinical Diagnostic Procedures.