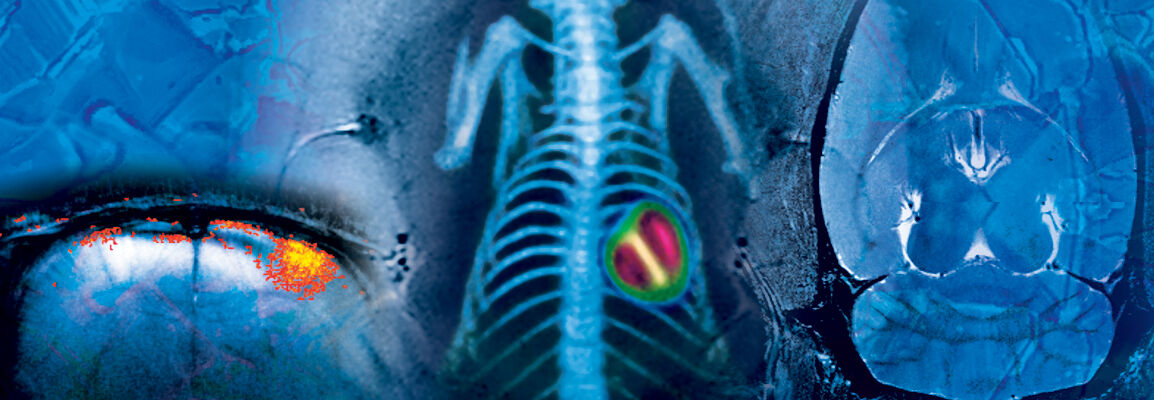
Preclinical Imaging
Preclinical imaging is a transformative platform that provides the only true in vivo translational approach to the clinic when it comes to monitoring profiles of disease manifestation as well as the impact of therapeutic intervention. By using the same technology and biomarkers of disease, both preclinically and clinically, can help accelerate decision making and build confidence in efficacy of treatment. Preclinical imaging has many advantages over conventional ex vivo tissue-based assessments where not only anatomical evaluations can be performed but also functional, metabolic, cellular and molecular readouts can be evaluated, often within the same animal. In addition, by imaging the animal longitudinally, more precise quantitative measures can be evaluated over time, providing profiles of disease, efficacy and toxicity effects within the same animal. This approach significantly reduces the total number of animals required for any one study helping to meet the best practices in animal research by adhering to the 3Rs principle (reduce, refine and replace).
Bruker supply the widest range of preclinical imaging systems including multimodality systems such as state of the art BioSpec MRI systems at the highest field strengths and sensitivities in the market that can be combined with or without PET for simultaneous or in line (Si78) measurements of radioligands, together with industry leading Skyscan portfolio of microCT and Si78 PET/CT or Albira Si PET/SPECT/CT trimodal systems. All these systems can play a pivotal role in assessing target validation, target interaction/lead optimisation, biodistribution/receptor binding of the molecule, pharmacodynamics and toxicology. Their utility is spans across all disease areas but particularly important when assessing chronic disease where multiple facets of the disease may manifest into the next stage and hence can be a crucial tool when assessing specific targets during the natural history of disease.
Our industry leading imaging systems not only provide the imaging technologies but also accessories and peripherals that optimise workstreams from the highest sensitivities associated with MRI such as our patented CryoProbe technology that provides a signal boost of between 3-5 fold as well as multimodal animal handling systems that can be used across all modalities.
Support
Service and Life Cycle Support
Bruker’s commitment to provide customers with unparalleled help throughout the buying cycle, from initial inquiry to evaluation, installation, and the lifetime of the instrument is now characterized by the LabScape service concept.
LabScape Maintenance Agreements, On-Site On-Demand and Enhance Your Lab are designed to offer a new approach to maintenance and service for the modern laboratory


