Novel Biomarker Predicts Doxorubicin Toxicity
“These findings provide the basis for noninvasive biomarker development of treatment response based on choline phospholipid metabolism”
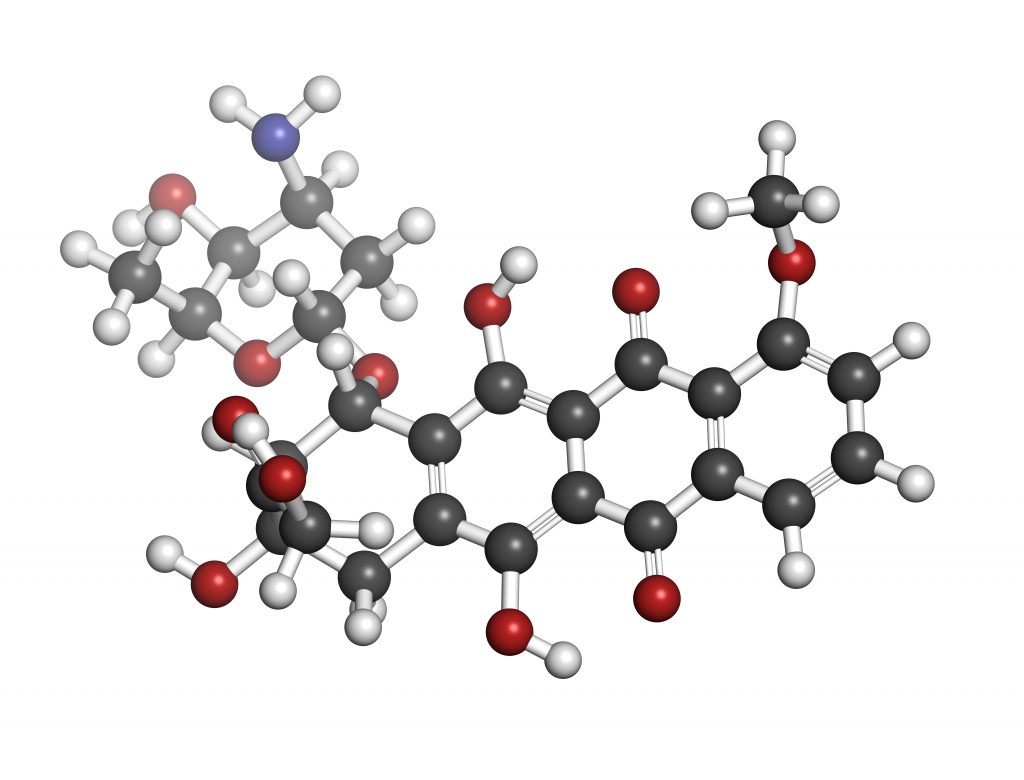
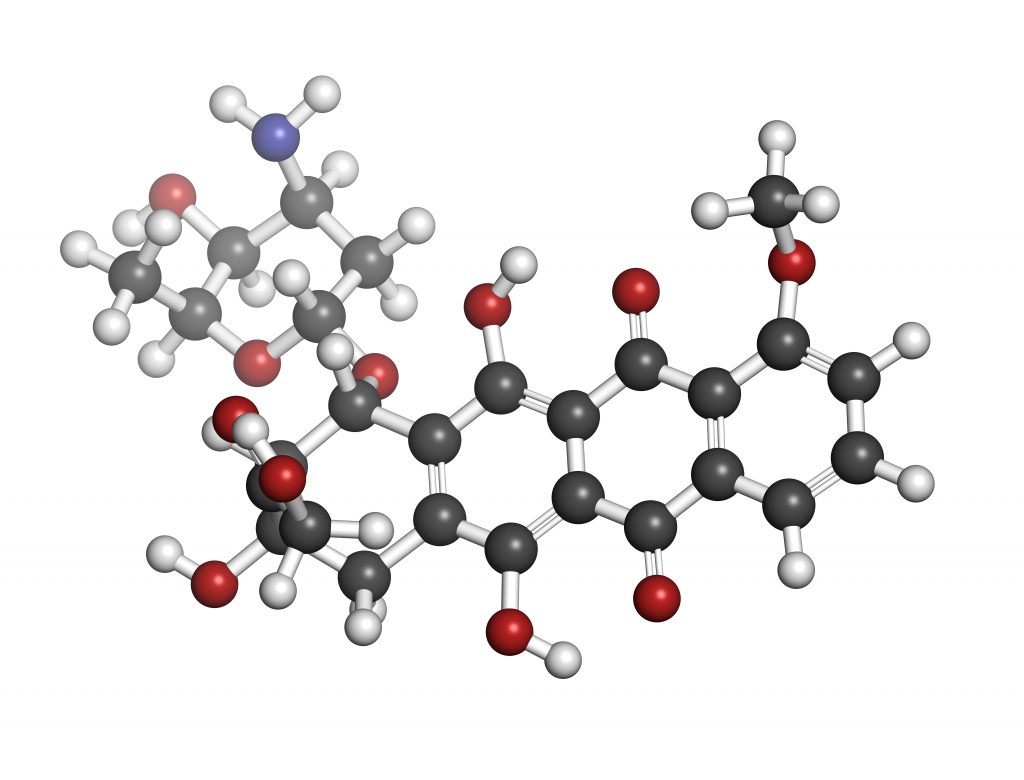
Recently, researchers used magnetic resonance spectroscopy (MRS) to identify specific markers of doxorubicin-induced side effects during breast cancer treatment, finding a way to block these negative effects and improve efficacy at the same time.1
MRS offers a precise method of determining the underlying chemical changes in a tumor, non-invasively.2,3 Non-invasive monitoring methods are easier, faster, and can be performed more often than biopsies for the determination of response rates in cancer patients. By better understanding the chemical components of a tumor, clinicians can use MRS to identify the type and grade of brain tumors, to follow treatment response, and to recognize recurrence in cancer patients.4,5
In order to better understand the mechanisms underlying doxorubicin efficacy and side effects, Dr. Menglin Cheng and colleagues at Johns Hopkins University in Baltimore, Maryland, treated two breast cancer cell lines (estrogen receptor positive (ER+) MCF7, and triple negative MDA-MB-231) with doxorubicin, using clinically relevant doses. The authors then analyzed metabolic changes produced in treated cells by 1H-MRS using a Bruker Biospin spectrometer.
The researchers measured total choline (tCho) levels, which are elevated in cancers,6,7 as well as phosphocholine (PC) and glycerophosphocholine (GPC). High ratios of PC-to-GPC are known to correlate with increased cancer malignancy.8 The study found that incubation of cancer cells with doxorubicin resulted in GPC levels 3 times higher than those of control cells, while PC levels were halved, leading to an increased PC/GPC ratio.
Similar results were observed in both cell lines, which harbor distinct genetic backgrounds, implying a wide potential for application of these metabolic patterns as a marker of doxorubicin treatment response in breast cancer. Doxorubicin treatment also produced dose-dependent reductions in glycerophosphodiester phosphodiesterase domain containing 6 (GDPD6), phospholipase D1 (PLD1), and choline kinase α (ChKα) protein levels, which are upregulated in cancers and are involved in cell migration, invasion, and cancer progression.9-11
Using siRNA directed against PLD1, the authors increased the efficacy of doxorubicin killing cancer cells, specifically in the triple negative line, and not in ER+ cells. However, inhibition of PLD1 with VU0155069 increased doxorubicin toxicity in both cell lines. ChKα-targeted siRNA improved the anti-cancer effects of doxorubicin in ER+ cells, but not in triple negative cells, whereas GDPD6 siRNA resulted in elevated doxorubicin efficacy in both cell lines. GDPD6 silencing, unlike PLD1 or ChKα, mitigated the doxorubicin-induced side effect of increased cancer cell motility.
Doxorubicin is a widely used first line agent for breast cancer despite its significant toxicity.12 Over 250,000 new cases of breast cancer were diagnosed in 2017 and over 40,000 patients died as a result of the disease.13 The discovery of a new potential biomarker for reducing doxorubicin toxicity as well as identifying a novel target for the development of new treatments for breast cancer are significant developments.
References:
- Cheng M, Rizwan A, Jiang L, et al. Molecular Effects of Doxorubicin on Choline Metabolism in Breast Cancer. Neoplasia. 2017;19:617-627.
- Gadian DG. The information available from NMR. NMR and its applications to living systems. 2 ed. New York: Oxford University Press Inc. 1995;29–64.
- Beloueche-Babari M, Chung YL, Al-Saffar NM, et al. Metabolic assessment of the action of targeted cancer therapeutics using magnetic resonance spectroscopy. Br J Cancer. 2010;102:1–7.
- Bulik M, Jancalek R, Vanicek J, et al. Potential of MR spectroscopy for assessment of glioma grading. Clin Neurol Neurosurg. 2013;115:146–153.
- Nelson SJ. Assessment of therapeutic response and treatment planning for brain tumors using metabolic and physiological MRI. NMR Biomed. 2011;24:734–749.
- Moller-Hartmann W, Herminghaus S, Krings T, et al. Clinical application of proton magnetic resonance spectroscopy in the diagnosis of intracranial mass lesions. Neuroradiology. 2002;44:371–381.
- Hourani R, Horska A, Albayram S, et al. Proton magnetic resonance spectroscopic imaging to differentiate between nonneoplastic lesions and brain tumors in children. J Magn Reson Imaging. 2006;23:99–107.
- Aboagye EO, Bhujwalla ZM. Malignant transformation alters membrane choline phospholipid metabolism of humanmammary epithelial cells. Cancer Res. 1999;59:80–84.
- Foster DA and Xu L (2003). Phospholipase D in Cell Proliferation and Cancer11National Cancer Institute, and the institutional support from the Research Centers in Minority Institutions (RCMI) program of the NIH. Mol Cancer Res 1, 789–800.
- Ramirez de Molina A, Rodriguez-Gonzalez A, Gutierrez R, et al. Overexpression of choline kinase is a frequent feature in human tumor-derived cell lines and in lung, prostate, and colorectal human cancers. Biochem Biophys Res Commun. 2002;296:580–583.
- Stewart JD, Marchan R, Lesjak MS, et al. Choline-releasing glycerophosphodiesterase EDI3 drives tumor cell migration and metastasis. Proc Natl Acad Sci. 2012;109:8155–8160.
- Minotti G, Menna P, Salvatorelli E, et al. Anthracyclines: Molecular Advances and Pharmacologic Developments in Antitumor Activity and Cardiotoxicity. Pharmacol Rev. 20104;56:185–229.
- American Cancer Society. Cancer Facts & Figures 2017. Accessed November 10, 2017. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf.

